Policing with Velvet Gloves

Joe Smarro, right, and Ernie Stevens of the San Antonio Police Department’s Mental Health unit.
By Anne Snyder
“We’ve got a lady that’s cutting herself with a knife right now.”
Officer Ernie Stevens looks at the laptop that’s blinking with this shift’s first call. His partner in the driver’s seat, Officer Joe Smarro, punches the address into the GPS.
“Hold her down until we get there. Then we’ll take over responsibility,” Ernie says into the phone.
Joe and Ernie are two of the six qualified officers that San Antonio’s police department deploys from its specialized mental-health unit. They go out in pairs, dress in plainclothes, and respond to crises that might be rooted in mental illness.
It’s easy to see they’ve bonded, having tag-teamed in the midst of high emotional intensity for over five years.
Four patrol cars are already parked at the scene, their strobe lights roving. “Yup, you can see how they’re responding,” Ernie says, exasperation latent in his tone. “Just because there was mention of a knife.”
The officers speak respectfully of their fellow patrolmen—jobs they once held—but it’s clear the pair operates from a broader definition of “disturbance.”
“All patrol sees in this call right here is ‘knife,’” Joe says. “So they’re immediately thinking in terms of tactics. It’s ‘I might have to get my gun out,’ or ‘I might have to shoot somebody.’
“But when I see this call, I see that this is someone who’s really having a bad day. This is someone who is really upset. Something’s happened in the last 24-48 hours that’s caused her to get to this point, to where she’s cutting herself. And chances are this is not the first time this has happened. We’re dealing with a cycle here, and something’s caused this cycle to resurface. We need to figure out what’s going on.”
This type of psychological insight into a volatile situation is the end result of a decade of retraining by San Antonio’s police force.
As the rest of the country remains embroiled in a heated debate on criminal justice, the city of 1.4 million has quietly reached the forefront of police reform by prioritizing mental-health-centered approaches and gaining the trust of its residents and public-service providers.
Since 2005, San Antonio has required its entire police force to enroll in a weeklong program called Crisis Intervention Training (CIT), which helps officers better understand and respond to the nuances of mental illness. It’s also helped sponsor a 37-acre treatment center to handle civilians in various stages of mental illness and substance abuse, giving those being diverted away from jail support in managing their challenges.
On this particular call, Joe and Ernie enter the house and move past the armed officers. There’s a woman on a couch, crying. A man shifts awkwardly in the kitchen. Joe walks up to him as Ernie goes toward the woman.
“OK,” Ernie says as he sits down catty-corner from her. “You’re Jessica? What’s going on? My name is Ernie.”
She struggles to catch her breath, looking wary and spent.

Officer Ernie Stevens looks as a woman reveals the marks where she cut herself, in her home in San Antonio, Texas. Stevens sat and spoke with the woman about what motivated her to injure herself and her possible suicidal thoughts before asking the woman if she wanted to receive further treatment at a mental-health facility built to temporarily treat the mentally ill outside of jail and outside of the ER. MATTHEW BUSCH
Jessica offers Ernie an agitated list of expletive-laced complaints about her boyfriend’s transgressions during an eight-year relationship. She unleashes anger and exhaustion in equal measure. Ernie stays calm, focused on her.
“I can see you’re upset,” he says. “Let me ask you something. One piece of information we received was that you were cutting yourself. Was that—…”
“I told you before that I did,” Jessica cuts him off with defiance, lumping Ernie in with the patrol officers who first reached her house.
“I’m sorry,” Ernie says softly. “Did you try to cut yourself today?”
“No.” She swallows convulsively.
“OK. Have you ever received any kind of counseling or therapy in the past?”
“I used to,” Jessica says. She says she was raped at age 18 and became pregnant. Her foster parents took her off meds to protect the baby, and the only thing she’s tried since is marijuana.
“So you feel overwhelmed?” Ernie asks. “Would that be fair to say?”
Jessica nods.
“OK” Ernie says. “Would you agree with me if I said, honestly, you don’t want to kill yourself, you just want this pain to go away?”
Jessica nods, gulping. She explains that she used to cut her legs, “just so I could feel better.” She openly accuses her boyfriend of sleeping with another woman when she is out of the house and of making her and the kids stay away from morning until 6 p.m.
She’s a gushing faucet of pain, but Ernie keeps his focus.
“OK, all right,” he says. “I can see that point of view. What I’m worried about is the way that you handle these types of stressors in your life. When you’re up against a crisis like this, and something happens, how are you equipped to deal with it?”
Jessica explains that she usually leaves and goes to a friend’s house, that she could never afford counseling and is afraid of its conditions.
“They tell me that if I’m going to harm myself…” her voice dwindles off. And then, “I don’t want them to take my kids away.”
Ernie responds swiftly.
“Let me put that fear at ease, OK? Hear me: There’s no way at all that I’m going to even consider taking your children away from you. All I want to do is get you help so you’re equipped to deal with life when it comes at you like this.”
The conviction in Ernie’s promise seems to break through to Jessica.
“Well, then, if someone’s going to check me, can I be honest with you and show you what I did?”
Ernie nods, having waited, it seems, for this breakthrough. Jessica stands up, takes off her outer shirt and lifts the camisole underneath. Ernie sighs heavily. Her chest is covered by a jigsaw puzzle of 50 bleeding gashes, some of them deep.
“Did you show the patrol officers this?”
“No,” Jessica says.
Ernie’s eyes narrow as he leans closer. “Let me see this for a second. They may want to suture these and put a couple of stitches in there. We need to get help. This is something we don’t want you to do. They can take care of this at the crisis center.”
Then he looks into her eyes.
“Listen to me, Jessica. I’m heartbroken. If you were my wife, my sister, I’d be heartbroken.”
Her eyes well up, hearing a truth about her value that’s been buried. And then…
“This is normal for me,” she says limply.
“Originally, I didn’t want to get into this line of work,” Ernie says back in the patrol car, after Jessica has been checked in to the crisis center, called Restoration.
“Dealing with a mentally unstable consumer was my biggest fear. I’d been a patrol officer for 13 years when a buddy signed me up for this training, called CIT. I just said yes because to do it would mean I’d get a weekend off.”
CIT was at that time new to San Antonio, having been introduced in 2005 as part of an initiative Bexar County was undertaking to stave off fines from an overcrowded jail.
A constellation of fresh municipal leaders came on the scene in the early 2000s—including the director of mental-health community services, a new police chief, and a new county judge (who had previously been San Antonio’s mayor)—and put their heads and political skills together to launch a deep listening effort between law enforcement officers and mental-health professionals. The idea was to get these two cultures to better understand one another and then hone in on what could be done to stop the cycle of incarceration for mentally ill persons.
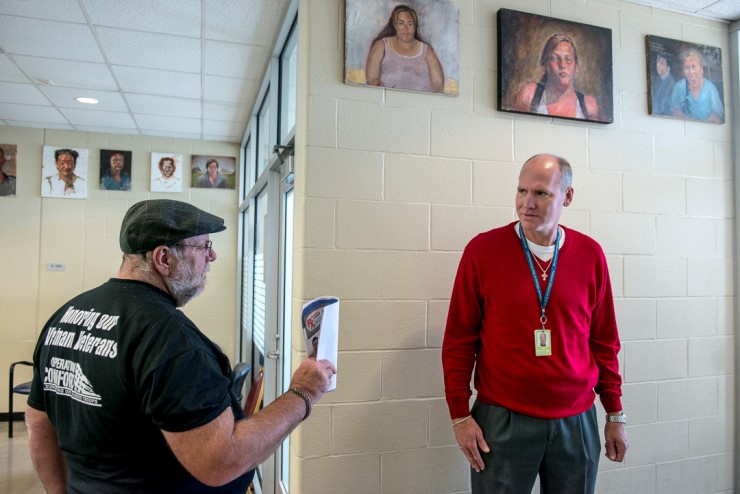
With the help of a six-person mental-health squad, San Antonio has diverted more than 100,000 people away from jail or emergency rooms into appropriate treatment—all without the use of force. MATTHEW BUSCH
Some time into these conversations, it became clear that the needs of the first responders—e.g. patrolmen and women—had to be prioritized. Mental-health and law enforcement leaders originally thought they could build mental-health services inside the jail. This proved ineffective: Too few inmates were being removed. So instead they targeted the most common transition vehicle for those with mental illness: squad cars.
Up to that point, police academies were not offering courses in how to deal with mental-health crises. Though officers often experienced an average of one such crisis per day while on duty, most settled for fumbling their way through the “crazies,” preferring a quick jail booking to the murkiness of a mentally ill person’s world.
“As soon as I got [to CIT], I did not want to be there,” Ernie remembers as we drive to the next crisis call, this one from a mother who says her 17-year-old son is threatening to harm himself and her. “I didn’t feel comfortable.”
Besides unease when faced with unpredictable psychoses, there was also the fear of being labeled a “hug-a-thug” or “social worker.” Ernie had been trained to be tough, to command and control. But on the fourth day of the training, he was introduced to an older woman named Jeanine who described what it was like to live with a schizophrenic son. Her testimony was riveting.
“‘One day, one of you officers will have to come to my house and you might have to shoot and kill my son,’” Ernie recalls her saying, still shaking his head at her resignation. “‘And I want you to know that if that happens, that’s OK. Because I want you to go home safe to your families. You don’t know what it’s like to live with this.’
“At that moment, everything changed for me,” Ernie remembers. “To see her resolved to the fact that her son would eventually be killed by a police officer, and to know she couldn’t possibly be alone … I just thought, there’s no way that this can be.”
For Joe, remorse also set in quickly after joining.
Nightmares haunted him for the first couple of months; taking on seven or eight mental-health calls per day disturbed his sense of reality. But perspective gradually returned as he and fellow officers recognized patterns in their calls and their discretion in maneuvering crises grew in deftness and sensitivity.
With the help of Joe, Ernie, and the rest of what is now a six-person mental-health squad, San Antonio has diverted more than 100,000 people away from jail or emergency rooms into appropriate treatment—all without the use of force.
We get out of the car, about 10 minutes after leaving Jessica safe at the crisis unit. Another woman is crying, this one in a dilapidated parking lot, darting her eyes to find her hooded son who is schizophrenic and allegedly threatening violence. Joe walks up to get more information from her as Ernie rounds the corner and carefully approaches the client.
“Hi, Victor? What’s going on? My name is Ernie.”
The success of San Antonio’s jail-diversion program has attracted national attention, and those who visit from other jurisdictions often walk away thinking Crisis Intervention Training is a magic lever to be implemented everywhere. There’s a striking humaneness to these officers, a nuance to their ability to build trust with those in the throes of crisis that makes this outside impulse understandable, especially in the current climate of anger towards police behavior.
Without robust treatment services also available, however, even a CIT-trained police force will have no choice but to wait 8-14 hours in an emergency room, or to book the person in the local jail.
When Ernie and Joe dropped off Jessica at the Restoration crisis unit, they knew they were ushering her into an array of resources, whether or not she ultimately decided to pursue treatment. Located just northwest of downtown, Restoration is a fully outfitted crisis-care and recovery center run by San Antonio’s Center for Health Care Services (a quasi-government agency focused on mental-health and substance-abuse solutions), adjacent to a 37-acre campus called Haven for Hope that provides longer-term residence and medical and behavioral care for the homeless, addicts, and the mentally ill.
When someone like Jessica is brought in by law enforcement, her case-management needs are assessed. Is mental illness co-occurring with substance abuse? Will she need to see a psychiatrist right away? What are all the challenges to her getting and maintaining access to treatment? Is it child care for her children? Is it food stamps? What is her relationship with her peers, coworkers, and family?
“We don’t want to be the end-all and be-all for everybody,” says Kathleen Doria, a contract employee at the Center for Health Care Services. “But what resources can we be the liaison for to keep this fragile case management together?”
Jessica looked both nervous and relieved as she waited for the verdict on her case. Journalists are not allowed to interview clients once admitted, but Ernie says it’s likely she was placed in the Josephine Recovery Center, Restoration’s 16-bed crisis residential and respite facility for men and women, which is focused on providing critical coping skills to sustain functioning and reintegrate into the community. What she does after that is up to her.
“I fear she’s going to go back to that same situation because she feels like she’s trapped in it,” says Ernie, as he relives the 15-20 minutes he and Joe spent de-escalating her crisis at home. “This may be a Band-Aid on an open wound for her. There are resources in place to help her, but she’s got to be willing to up and leave [her current situation].”
This struggle to achieve proper agency is what the rest of the Center’s wraparound services are designed to support. From its crisis-care unit and recovery center, to its Mommies Program that treats pregnant and parenting women who use or abuse substances, to its sobering and detoxification programs and an integrated primary-care clinic complete with counseling and therapy services, all of the programs are in one location. Many staff members are “peers” who once found themselves in similar straits, and attend alongside patients to offer legitimate empathy and a glimpse of what’s possible.
The common thread that binds all the available tracks—including Haven for Hope’s more intensive 90-day treatment for homeless and mentally-ill patients—is an orientation toward empowering the patient, to get her in the driver’s seat of her recovery.
Scott Ackerson directs Haven for Hope, across the street from Restoration Services, and he’s convinced that this person-centric approach needs to precede tactical checklists. “I’ll ask a patient, ‘What do you live for?’” Ackerson says. “A common response is, ‘I want to get my kids back.’ OK, then that’s your goal. Your goal is not medication compliance. If you have issues with mental illness or addiction, do those need to be addressed? Absolutely. But that’s not your goal. Your goal is to get your kid back…. The only way a person can recover is if they’re wanting and willing to recover.”
This drilling-down into the needs and identities of people who have been stripped of their scaffolding is the philosophical and cultural strain that seems to run through every piece of San Antonio’s learned-intervention and treatment strategies. There’s a striking consistency to the way Joe and Ernie listen and speak when they’re on a call, to the way the nurses and directors of Restoration’s crisis unit listen and speak, to the way Scott in longer-term care listens and speaks. They focus on relationships, listening deeply, and want to help each person recover a sense of his or her true self.
San Antonio is not slowing down in leveraging what’s worked in creating an unusual continuum of care from police intervention to treatment and recovery. This next year, the city plans to permanently remove 400 jail beds in order to create another 400 beds for the Center for Health Care Services’s treatment programs. So far, the Bexar County jail has emptied 500 beds since the diversion program began. In the last year alone, from Dec. 21, 2014 through Nov. 30, 2015, the Center for Health Care Services estimates that 9,270 individuals have been diverted from jail.
The push for ongoing improvements is rooted in a confidence that the unique collaborative culture developed across San Antonio’s public-service sector will continue to bear fruit. Leadership has been significant—motivated doers seeing the same problem at the same time—but a city ethos of non-territoriality and cross-sector appreciation has been the mortar allowing for ongoing gains.
Most notably, a police force is experiencing a very real sea change in mind-set and disposition. The quiet passion of Joe and Ernie has not only earned the respect of their fellow officers, it’s provided a needed safety valve for mentally unstable policemen and women within the department. In a year of heightened national scrutiny on the powers and preparedness of law enforcement, the pair once ridiculed for their “hug-a-thug” skills are now leaned upon for their ability to listen and provide counsel for the psychoses that may be burdening their colleagues on patrol. Lives have arguably been saved as job posts are now attached to a peer-to-peer web of psychological support.
Whether other cities will successfully adopt San Antonio’s approach depends somewhat on those local cultural entrenchments that precede the extent of the incarceration problem. Racial dynamics, a city’s size, the precedence of cross-sector collaboration, and the will to invest in wraparound treatment services are all variables that can affect each jurisdiction’s chance of emptying jail beds and reducing deaths. But for now, San Antonio’s lessons are worth studying. In a racial and criminal-justice debate defined by heat, this growing Lone Star city provides some light.
Update: This story has been edited to reflect that Kathleen Doria is a contract employee of CHCS, not a spokesperson.
This article was originally published by the National Journal on 1/21/2016









